Since last summer this conversation has used comparative change in covid hospitalizations to assess the demand implications of the pandemic. I treat hospitalizations as the most consequential “pull” factor — certainly on the health care system, but also on economic life. Hospitalization is also a leading indicator for deaths.
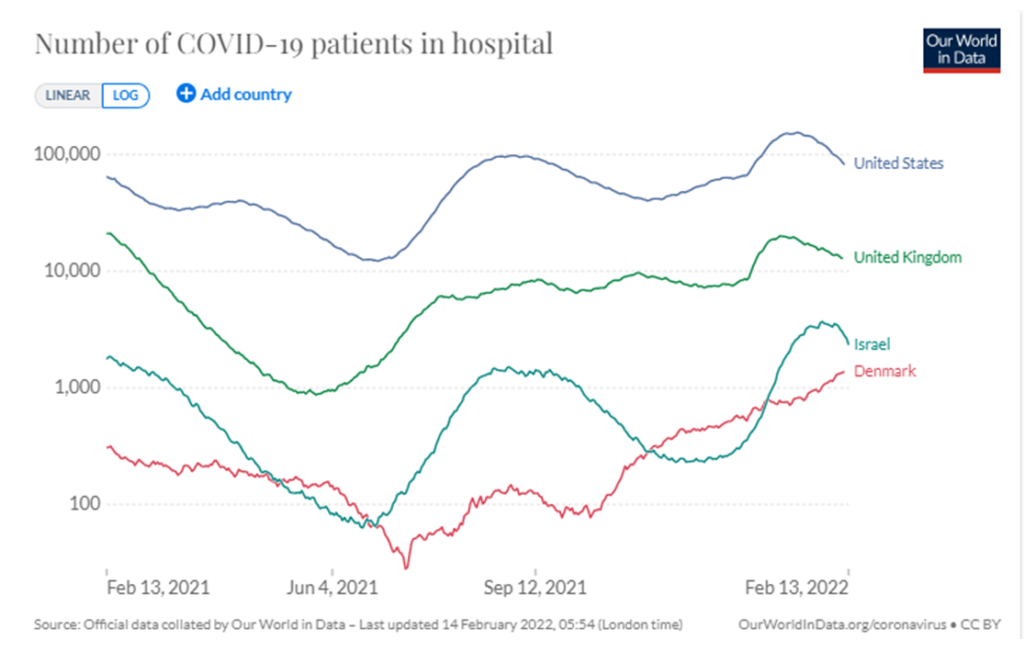
I have focused on four demand curves: United States, United Kingdom, Denmark, and Israel. I live in the United States as do most of my readers. The other three nations have health surveillance systems considerably more comprehensive and integrated than the United States. So far in the pandemic, one or more of these three nations has served as an accurate bellwether of where demand curves in the United States (and elsewhere) will go in another few weeks.
Below is the comparison as of February 13 (and over the last twelve months). All four nations currently have some of the highest hospitalization counts since the pandemic started. Three of four, however, appear to be undergoing a sustained reduction in hospitalizations. The fourth, Denmark, still has increasing hospitalizations, but has decided there is sufficient health-care supply for the current level of demand. The omicron wave has killed tens-of-thousands, but has also presented a less deadly proportional threat per total transmissions. Most nations now report declines in hospitalizations. But Denmark is not alone, Japan is now at least seven weeks into a surge of covid cases and hospitalizations.
What comes next with covid is unknown. Vaccinations and prior infections are constraining viral effects. Improved therapeutics are reducing morbidity and death. Mutation is ongoing. History demonstrates that pandemics can persist or recur for decades. The context for covid is unprecedented. The global population for the 1918 pandemic was less than 2 billion. There were still fewer than 3 billion for the 1957 pandemic. There are now about 8 billion people and we are much more mobile than ever before. Humans now provide much higher potential velocity for mutations and infections.
We are probably conditioned by evolution to discount risks that are less than imminent. So, as the most recent covid wave fades (slightly, per the chart below), there is clearly a desire to “get-back-to-normal.” This preference is understandable and related behavior can even be constructive. As a mind-set or risk-management strategy, however, such preferences are at least premature and potentially dangerous.
Here’s just one scenario that suggests remaining vigilant: The comparative success of China’s zero-covid strategy (more and more) could, paradoxically, increase its vulnerability to future coronavirus mutations. Given the size of China’s population and the key role the nation plays in the global economy, what goes wrong in China does not stay there.