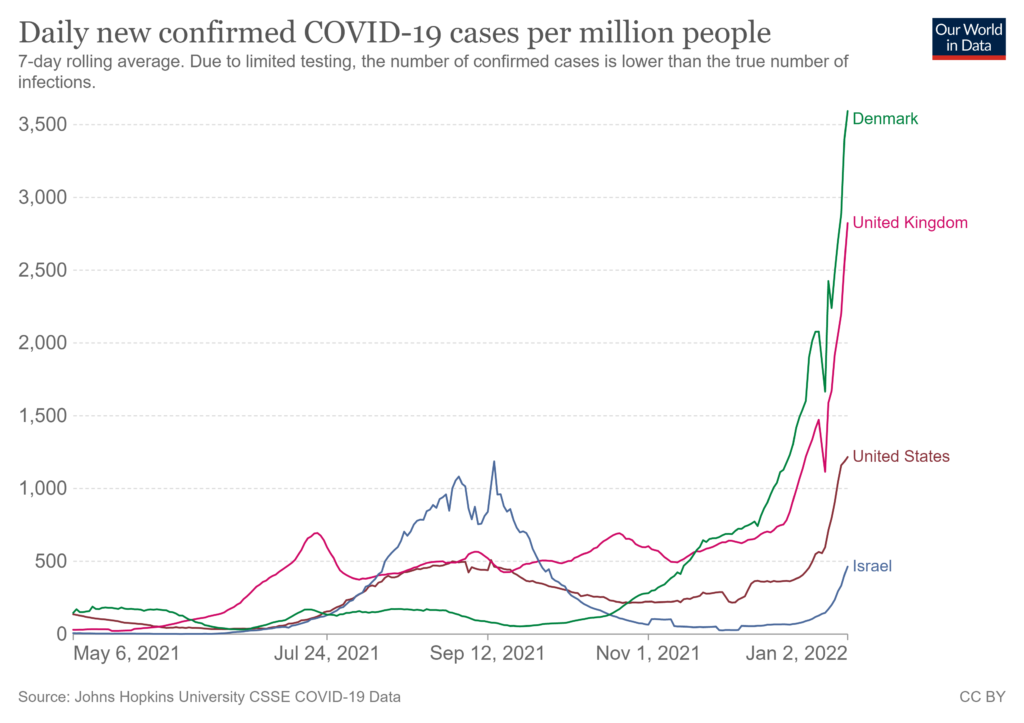
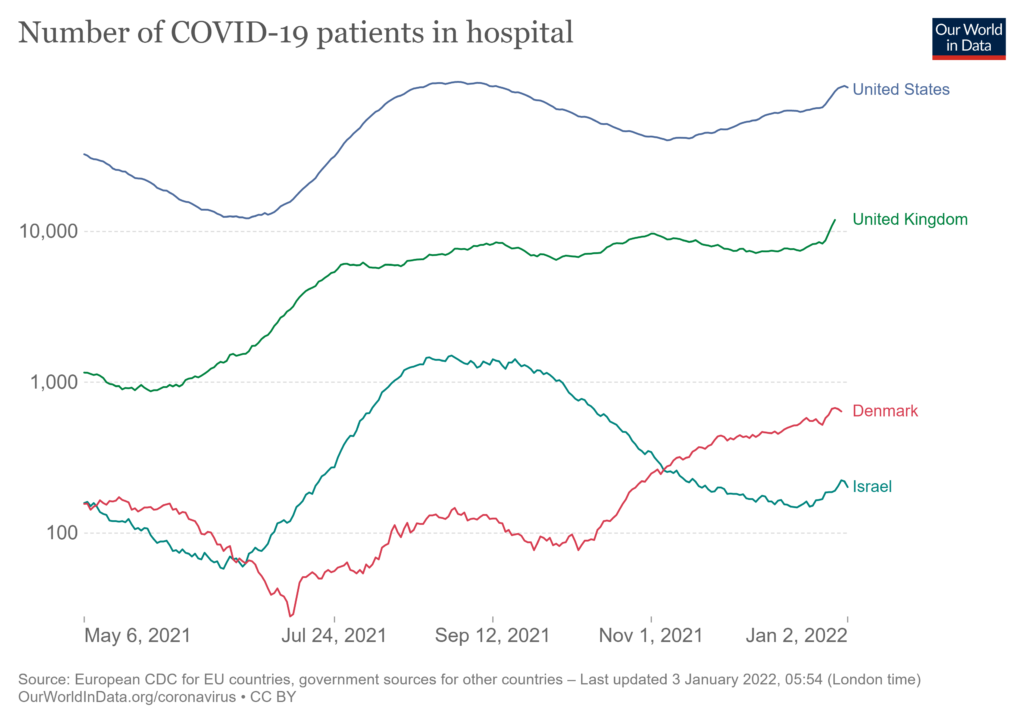
“This is not the same disease as we were seeing a year ago,” according to Sir John Bell, professor of medicine at the University of Oxford, discussing the omicron variant’s impact on covid. Infections are skyrocketing (see first chart below), but symptoms are often milder and hospitalizations — while rising — are increasing at a much lower rate than with prior dominant variants (see second chart below).
The data subtext for these case counts can be treacherous. Israel and Denmark have sophisticated real-time data-streams on new cases. UK data sources are almost as good. US case counts are much less accurate, especially after a long holiday. But Denmark’s sudden surge last week reflects social behavior and easy access to testing as much as infection rates. Especially in the context of omicron, hospitalizations are a more confident comparative measure.
Risks to the healthcare system — and other crucial networks — continue to be significant. While hospitalization rates are much lower, infections are much higher. The lower rate can still generate significant new admissions. Many US hospitals are already short-staffed. Several key supply chains have been struggling to keep and recruit sufficient workforce levels before omicron emerged (more). Strict adherence to isolation and quarantine guidance could decimate flow capacity.
Widespread omicron contagion can now be assumed. Spread and depth of disease is still to be seen. Cascading impacts on supply chain capacity should roughly track disease penetration across the population. Watching how, when, and where constraints on flow emerge may provide helpful hints on potential mitigation measures. This is what I will watch and update here over the next three or so weeks.