Last week an earnest well-intended political leader said, “All it takes to beat this virus and return to normal is getting shots in arms.”
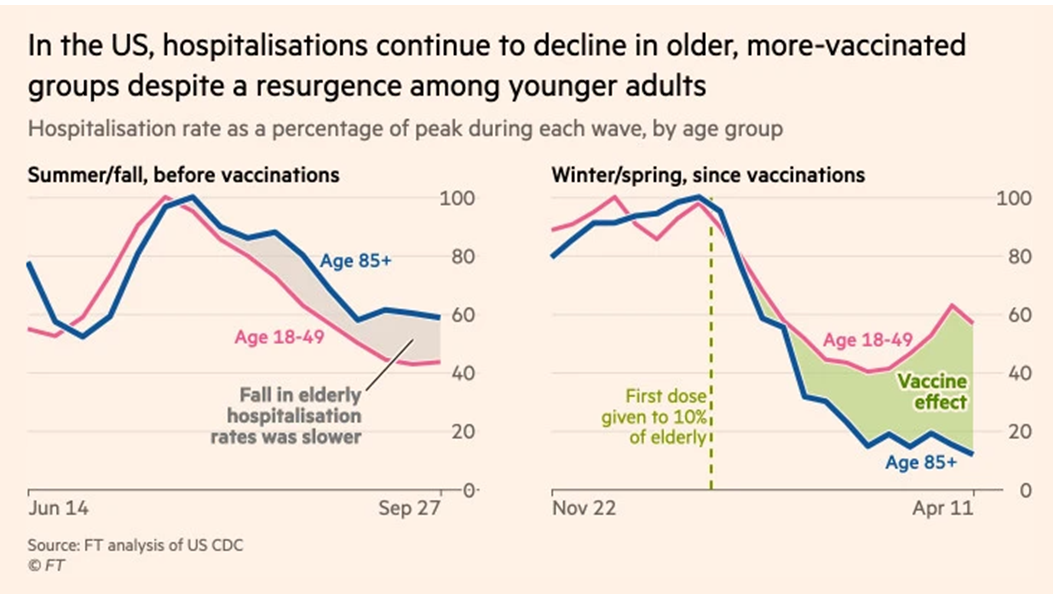
It is tempting to make this claim. Mass vaccinations are making a positive difference. The closer we get to or beat 80 percent vaccination rates, the less our risk of wide-spread recurrence of deadly disease.
But if “normal” is meant to suggest a near-term context where coronavirus is no longer a risk, this claim is over-stated.
In April 2020 tight containment and even eventual eradication of SARS-CoV-2 might still have been possible. But since then the virus has had too much opportunity to spread, strengthen, and diversify. Today it has hundreds-of-millions of use-cases for evolutionary test-drives. Most mutations will be minor and meaningless. But the virus now operates at a scope and scale where supercharged evolutionary tweaks cannot be discounted.
Given this risk it is not prudent to promise a return to normal even with the recent rate of US vaccinations, and unfortunately the recent rate is slowing.
We can credibly claim much lower risk by preparing Americans for another year — probably two — featuring five fundamental risk-management practices:
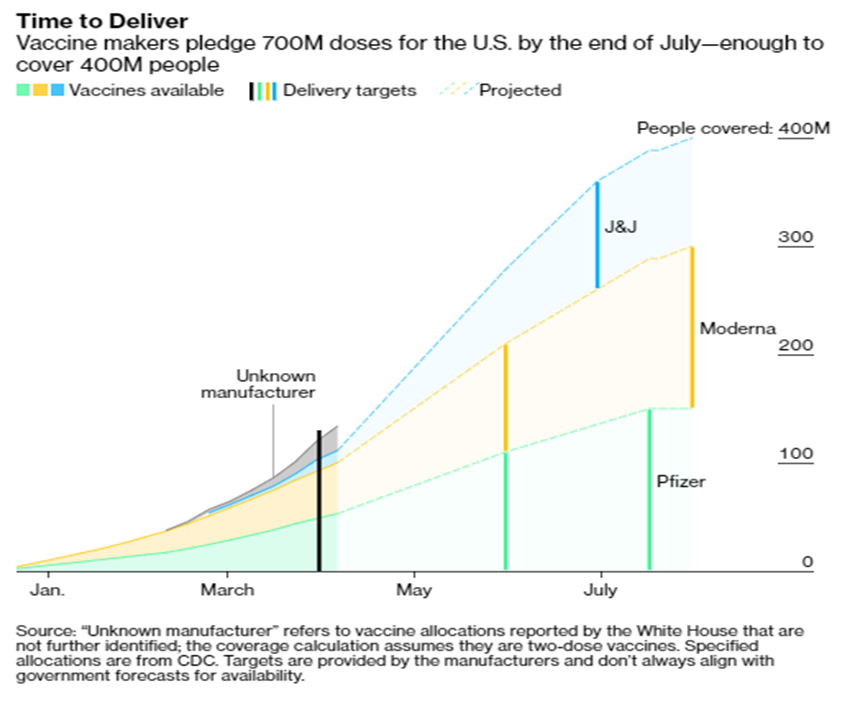
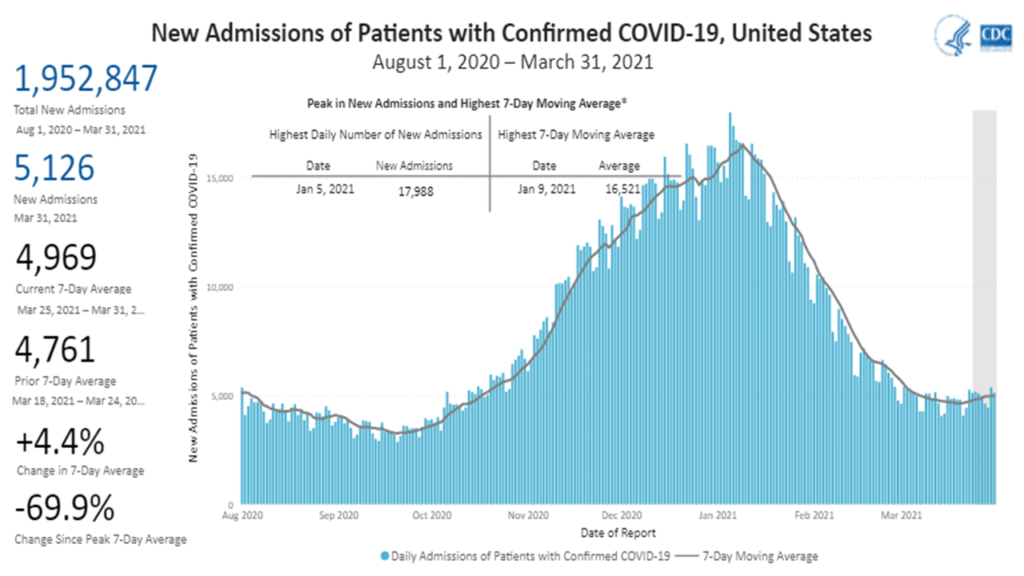
Vaccinate: As of April 25 just over 42 percent of all US residents (53 percent of those over age 18) have been vaccinated. This is already slowing viral flow in the United States. But for sustainable impacts on transmission and to slow mutations we need vaccination rates above 70 percent, the higher the better. We are still not making enough targeted and systemic investments — financial and otherwise — to encourage and facilitate vaccinations. We should also anticipate the need for booster shots on some yet to be determined cycle.
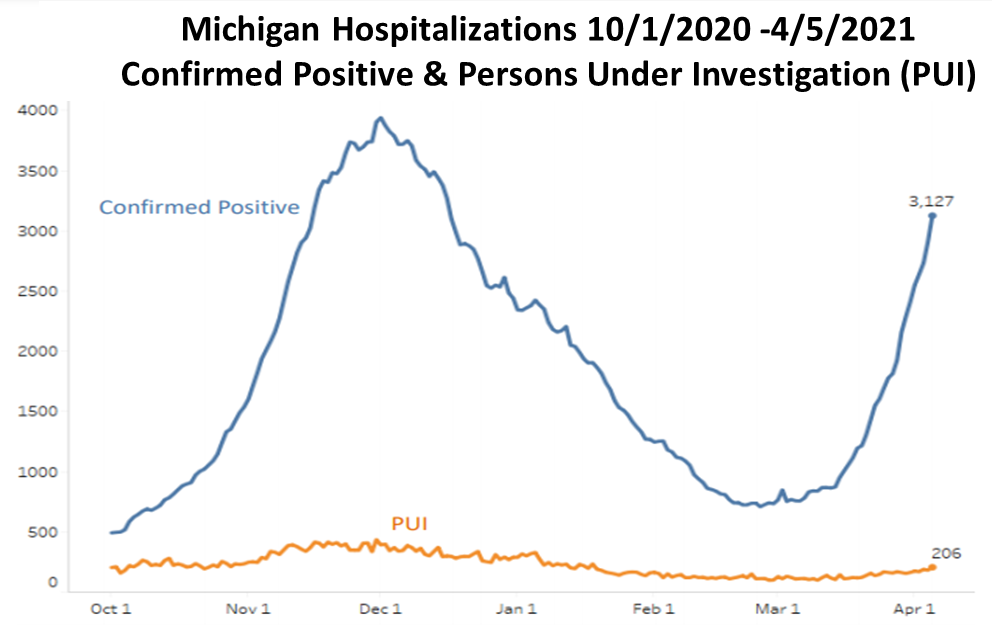
Test, trace, and contain: If twenty percent of US residents remain unvaccinated that is more than 60 million mobile mutation manufacturers scattered around the country. Among the vaccinated, demonstrated efficacy ranges from 72 to 96 percent depending on which vaccine and the profile of the vaccinated person. As a result, entirely domestic transmission and evolution of the disease will continue. These risks can be mitigated if local outbreaks (especially of new variants) are identified and effectively engaged as early as possible. This requires a much more robust multimodal testing and tracing capacity than the United States has so-far developed. South Korea continues to set the pace for testing/tracing. For cultural and constitutional reasons the South Korean model is problematic for the United States. But plenty of more targeted methods have been proven effective.
Support global mitigation: In addition to plenty of native-born variants, the B.1.1.7 variant, first identified in the United Kingdom, has accelerated transmissions and increased covid cases in the United States. Other variants have (and will) spread. The more the United States can do to suppress viral flames elsewhere, the less risk of heat-stroke or much worse here.
Reduce overall circulation: The coronavirus thrives on meeting new people in new places. Even vaccinated people — given significant but less than 100 percent viral suppression — are potential sources of transmission. Until vaccination rates exceed 70 percent and testing/tracing is much more extensive we should minimize our circulation. (Please see this and this and this.) I am guessing we need about 25 to 35 percent below pre-pandemic circulation to have a substantive impact on viral transmission. Today the United States has a national average of about 15 percent below pre-pandemic mobility levels.
Avoid interior crowds: Hand hygiene, physical distance, and masks help. But the most fertile sources of virus transmission have been over-crowded, badly ventilated, interior spaces. The more time spent with more people in any enclosed space, the higher our risk. Less time, fewer people, better ventilation (more), or staying outside is the healthier choice.
The risk of covid-related disease and death will persist. As we are seeing in Brazil and India — and can vividly recall from Wuhan, Bergamo, Queens, and perhaps your hometown — there is a very real — sometimes sudden — risk of healthcare systems being overwhelmed. In the next few years we are unlikely to eliminate the risks of covid. But we can now limit these risks to a level that will not threaten the US healthcare system. This will ensure quality care for those hospitalized and reduce wider health and economic effects.
The five fundamentals outlined above require continued investment in public health, shared discipline, and some personal restraint. Systemic failure to observe these fundamentals is likely to result in unnecessary disease, death, economic dislocation, and social turmoil. As always, we make choices.